A cataract is a clouding or opaque area over the lens of the eye–an area that is normally transparent. As this thickening occurs, it prevents light rays from passing through the lens and focusing on the retina–the light sensitive tissue lining located in the back of the eye. This clouding is caused when some of the protein which makes up the lens begins to clump together and interferes with vision.
What causes cataracts?
Although scientists do not know for sure what causes cataracts, they suspect there could be several possible causes including:
 Smoking
Smoking- Diabetes
- Excessive exposure to sunlight
- Steroid use
- Diuretic use
- Certain major tranquilizers
For several of the potential causes listed (for example, steroids, diuretics, and/or major tranquilizers), additional research is needed to differentiate the effect of the disease from the effect of the drugs themselves.
What Are The Symptoms Of Cataracts?
The following are the most common symptoms of cataracts. However, each individual may experience symptoms differently. Symptoms may include:
- Cloudy or blurry vision
- Lights appear too bright and/or present a glare or a surrounding halo
- Poor night vision
- Multiple vision
- Colors seem faded
- Increased nearsightedness, increasing the need to change eyeglass prescriptions
- Distortion of vision in either eye
 Often in the disease's early stages, you may not notice any changes in your vision. Since cataracts tend to grow slowly, your vision will worsen gradually. Certain cataracts can also cause a temporary improvement in close-up vision, but this is likely to worsen as the cataract grows. The symptoms of cataracts may resemble other eye conditions. Consult a doctor for diagnosis.
Often in the disease's early stages, you may not notice any changes in your vision. Since cataracts tend to grow slowly, your vision will worsen gradually. Certain cataracts can also cause a temporary improvement in close-up vision, but this is likely to worsen as the cataract grows. The symptoms of cataracts may resemble other eye conditions. Consult a doctor for diagnosis.
What are the different types of cataracts?
According to the National Eye Institute, part of the National Institutes of Health, cataract types are subdivided accordingly:
- Age-related cataracts. The majority of cataracts are related to aging.
- Congenital cataracts. Some babies are born with cataracts or develop them in childhood, often in both eyes. Some congenital cataracts do not affect vision, but others do and need to be removed.
- Secondary cataracts. Secondary cataracts develop primarily as a result of another disease occurrence in the body (for instance, diabetes). Secondary cataract development has also been linked to steroid use.
- Traumatic cataracts. Eye(s) that have sustained an injury may develop a traumatic cataract either immediately following the incident, or several years later.
Other sources, including the American Academy of Ophthalmology, describe the different types of cataracts according to the cataract location on the eye lens, including: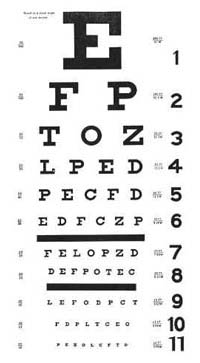
- Nuclear cataract. This is the most common type of cataract, and the most common type associated with aging. Nuclear cataracts develop in the center of the lens and can induce myopia, or nearsightedness–a temporary improvement in reading vision that is sometimes referred to as "second sight." Unfortunately, "second sight" disappears as the cataract grows.
- Cortical cataract. This type of cataract initially develops as wedge-shaped spokes in the cortex of the lens, with the spokes extending from the outside of the lens to the center. When these spokes reach the center of the lens, they interfere with the transmission of light and cause glare and loss of contrast. This type of cataract is frequently developed in persons with diabetes, and while it usually develops slowly, it may impair both distance and near vision so significantly that surgery is often suggested at an early stage.
- Subcapsular cataract. A subcapsular cataract usually starts as a small opacity under the capsule, at the back of the lens. This type of cataract develops slowly and significant symptoms may not occur until the cataract is well-developed. A subcapsular cataract is often found in persons with diabetes, myopia, retinitis pigmentosa, and in those taking steroids.
How are cataracts diagnosed?
In addition to a complete medical history and eye examination, diagnostic procedures for cataracts may include:
- Visual acuity test. The common eye chart test (see above), which measures vision ability at various distances.
- Pupil dilation. The pupil is widened with eye drops to allow a close-up examination of the eye's retina.
In addition, other tests may also be performed to help your eye care professional learn more about the health and structure of your eye.
What are the risk factors for cataracts?
Possible risk factors for cataracts include:
- Age. Probably the greatest risk factor for cataracts is age. And, although age-related cataracts may develop between 40 and 50 years old, vision is usually not affected greatly until after age 60.
- Geographic location. Recent studies have shown that people who live in high altitudes are more at risk for developing cataracts.
- Excessive sun exposure. People who spend more time in the sun may develop cataracts earlier than others. The American Academy of Ophthalmology now recommends wearing sunglasses and a wide-brimmed hat to lessen exposure to ultraviolet rays.
Treatment for cataracts
Specific treatment for cataracts will be determined by your doctor based on:
- Your age, overall health, and medical history
- Extent of the disease
- Expectations for the course of the disease
- Your opinion or preference
- Your tolerance for specific medications, procedures, or therapies
In its early stages, vision loss caused by a cataract may be aided with the use of different eyeglasses, a magnifying glass, or stronger lighting. When these measures are no longer helpful, surgery is the only effective treatment available, for most individuals. It is important to note that a cataract only needs to be removed when vision loss interferes with everyday activities, such as driving, reading, or watching television. You and your doctor can make that decision together.
What is involved in cataract surgery?
Cataract surgery is one of the most common operations performed and one of the safest and most effective. Surgery involves removing the cloudy lens and replacing it with a substitute lens. If cataracts are present in both eyes, they cannot be removed at the same time. Your doctor will need to perform surgery on each eye separately.
Cataracts are generally removed in one of two ways:
- Phacoemulsification (also called small incision cataract surgery). This most common type of cataract removal procedure involves the surgeon making a small incision on the side of the cornea–the clear, dome-shaped surface that covers the front of the eye–where a tiny probe emits ultrasound waves to soften and break up the cloudy center of the lens. The cataract is then removed by suction through the same incision.
- Extracapsular surgery. During this procedure, a longer incision is made on the side of the cornea to remove the hard center of the lens; the remainder of the lens is then removed by suction.
According to the National Eye Institute, in most cataract surgeries the removed lens is replaced by an intraocular lens (IOL). An IOL is a clear, artificial lens that requires no care and becomes part of the eye. With an IOL, a person has improved vision because light will be able to pass through the retina. The recipient of the new lens does not see it or feel it.
What is an "after-cataract"?
An "after-cataract" occurs when part of the natural lens not removed during cataract surgery becomes cloudy and blurs vision. Unlike a cataract, an "after-cataract" can be treated with a technique called YAG laser capsulotomy. In an outpatient procedure, the doctor uses a laser beam to make a tiny hole in the lens to let the light pass through. After-cataracts may develop months, or even years, after cataract surgery.